What is Isthmocele (Cesarean Scar Defect)?
An isthmocele (cesarean scar defect) is a defect resulting from the inadequate healing of the incision made during a cesarean section in women who have previously given birth.
An isthmocele (cesarean scar defect) is a defect resulting from the inadequate healing of the incision made during a cesarean section in women who have previously given birth.
An isthmocele (cesarean scar defect) is a defect resulting from the inadequate healing of the incision made during a cesarean section in women who have previously given birth. While isthmocele were rare before the widespread use of cesarean sections, they have become more common. Risk factors for the development of isthmocele after cesarean sections have not yet been established. Studies have investigated whether single-layer or double-layer closure of the uterus after delivery, and whether the uterine closure is performed with or without a locking suture, all of these factors have had an impact on the development of isthmocele. However, no method has been conclusively proven to increase or decrease the risk of isthmocele.
An isthmocele, or the incision made during a cesarean section that fails to heal properly and creates a defect, causes menstrual blood to fill this area and, after the menstrual period ends, the blood that has been trapped there to leak out intermittently through the vagina. This often causes patients to complain of continuing dark brown or black bloody discharge after their period ends. Continuing dark brown bleeding and spotting after menstruation negatively impacts the patient's comfort. Spotting that occurs when going to the bathroom, spotting that occurs after sexual activity, and prolonged dark brown or black spotting negatively impact the patient's daily life and psychological well-being.
While isthmocele can cause the problems listed above, they can also cause difficulties in achieving pregnancy in women who want to conceive. There are numerous studies and publications demonstrating that the chance of successful pregnancy, even with in vitro fertilization (IVF), is reduced in women with a previous cesarean section and isthmoceles. In other words, isthmoceles can be another cause of infertility in women who have had previous pregnancies and given birth.
If pregnancy occurs in the presence of an isthmocele, and the pregnancy implants in the area where the isthmocele is located, it can lead to life-threatening complications such as a cesarean scar pregnancy, placenta previa (the placenta implanting lower in the uterus), and placenta accreta (the placenta implanting deeper in the uterine wall and not separating after birth). In cases of isthmocele, the risk of the isthmocele opening and rupture before labor increases, potentially endangering the life of both mother and baby.
As can be easily understood from the above explanations, the presence of isthmocele is a condition that negatively affects the comfort of life in cases where pregnancy is not planned, can cause difficulties in conceiving and infertility in cases where pregnancy is planned, and brings vital risks for the mother and the baby in case of pregnancy.
The patient's medical history is crucial in diagnosing an isthmocele. The patient's history may include a previous Caesarean section, and prior to this surgery, menstrual periods were regular, lasting for a certain number of days before stopping. However, after the Caesarean section, brownish-black spotting appeared after the menstrual period ended, sometimes for a few days, sometimes until the start of the next period, when the menstrual flow was reduced, or after intercourse. In some women, the isthmocele is so large and the menstrual flow so scanty that they present to us with amenorrhea and are subsequently diagnosed with an isthmocele during examination.
In patients presenting with this history, an ultrasound performed during a gynecological examination reveals a fluid-filled, usually triangular-shaped structure, extending into the uterine wall at the site of the incision made during the cesarean section. This is known as an isthmocele. If the ultrasound is performed during menstruation, the probability of diagnosing an isthmocele is higher. If menstruation has ended and the fluid accumulating in the isthmocele sac has disappeared, the diagnosis of an isthmocele may be missed by ultrasound. In this case, fluid can be injected into the uterus to increase the sensitivity of the ultrasound. MRI (magnetic resonance imaging) and hysteroscopy are also methods used to diagnose an isthmocele. Hysteroscopy, which involves entering the uterus with a camera and visually viewing the isthmocele itself, also facilitates diagnosis.
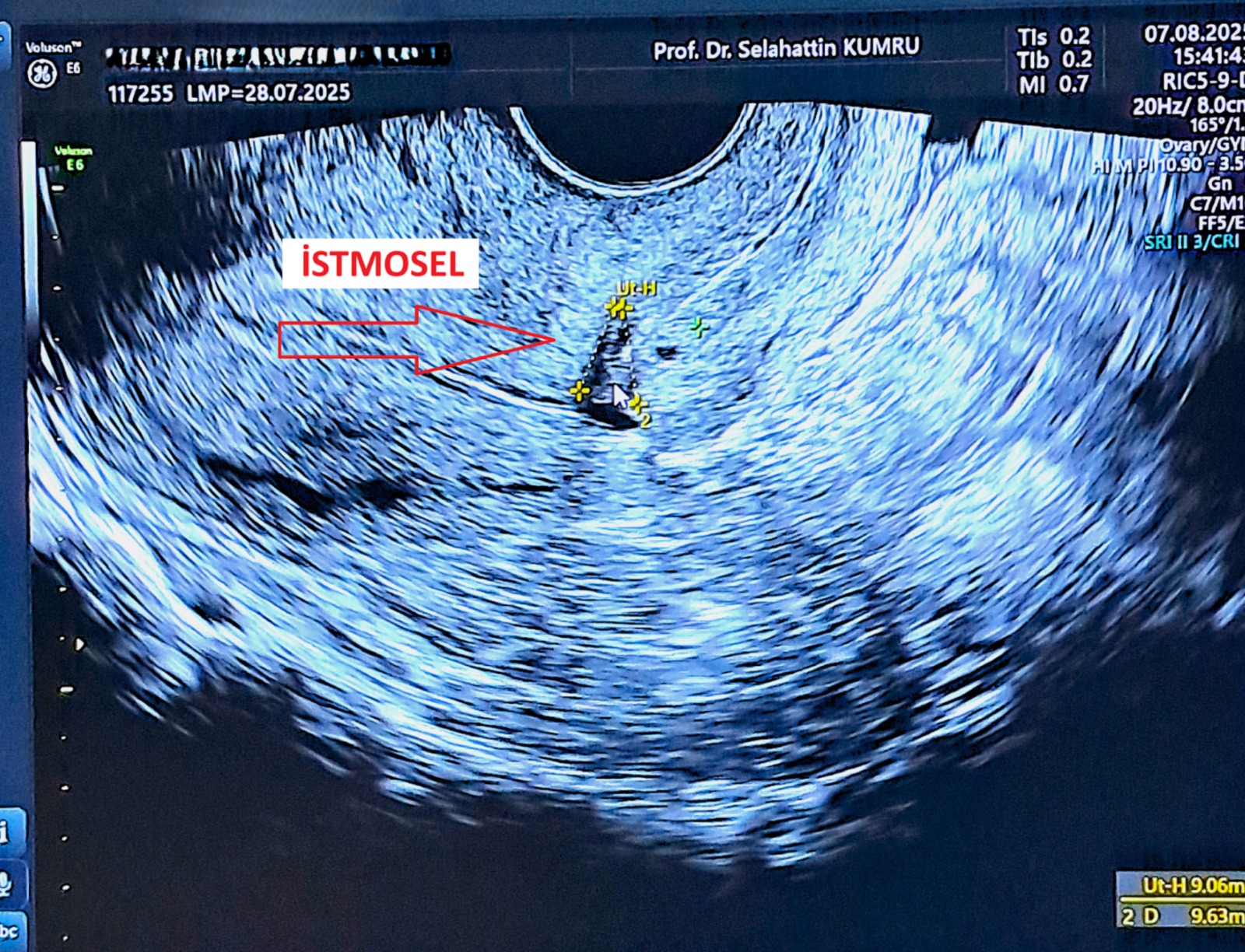
Ultrasonographic view of an isthmocele diagnosed in our clinic.
Once an isthmocele is diagnosed, treatment varies depending on the patient's symptoms and expectations. The goal of isthmocele treatment is to eliminate the defect in the area where the isthmocele is located and prevent menstrual blood from accumulating there. This can be achieved in two ways. One of these is a hysteroscopy, which involves entering the uterus with the aid of a camera, visualizing the isthmocele defect, and filing down the defect above and below to prevent blood accumulation. This prevents menstrual blood from accumulating in the isthmocele sac and, since there is no blood left there after the menstrual period ends, subsequent spotting is prevented. Hysteroscopy for isthmocele is a non-invasive procedure that may be preferred if the patient is not planning a future pregnancy or if the uterine wall is sufficiently thick in the area of the isthmocele. However, if the patient is planning a future pregnancy and the uterine wall in the area of the isthmocele is not thick enough, repairing the isthmocele with hysteroscopy will weaken that area and may lead to ruptures in that area of the uterine wall in subsequent pregnancies. In such cases, the isthmocele should be repaired intra-abdominally.
Isthmocele repair can be performed intra-abdominally, as in a Caesarean section, or by camera-assisted laparoscopy. If the abdominal isthmocele is repaired intra-abdominally, as in a Caesarean section, the incision made during the previous Caesarean section is reopened and re-sutured. The risks of this surgery and the post-operative return to daily life are similar to those of a Caesarean section. Laparoscopic isthmocele repair involves a camera-assisted incision into the abdomen and the incision is made in the area where the isthmocele is located. The incision is made until healthy tissue is exposed. Any dead tissue is removed, and once healthy tissue is recovered, the area is then re-sutured. The complications, risks, and return to daily life of laparoscopic isthmocele repair are similar to laparoscopic surgery, and compared to open surgery, the post-operative discomfort and pain are shorter and less severe. In our clinical practice, if we decide to repair the isthmocele intra-abdominally rather than hysteroscopy, we generally plan our surgery as a laparoscopic procedure. Laparoscopic isthmocele repair is a very comfortable procedure for the patient, but it requires experience and effort for the physician.